Nerve-Sparing Intracostal Rib Retractor
Redesigned thoracotomy retraction to eliminate the root cause of chronic post-surgical pain by avoiding intercostal nerve compression.
Overview
Post-thoracotomy pain syndrome (PTPS) affects over half of patients undergoing open lung surgery, often persisting for months or years and significantly degrading quality of life. Despite advances in minimally invasive techniques, rib retraction itself has remained fundamentally unchanged for decades—continuing to compress the intercostal nerve during surgery.
This project set out to answer a simple but powerful question:
What if ribs could be spread without ever touching the intercostal nerve?
The result is a nerve-sparing intracostal rib retractor that achieves surgical exposure while eliminating direct nerve compression—the leading cause of PTPS.
The Problem
Open thoracotomy remains the gold standard for lung cancer resection, requiring mechanical rib spreading for access to the thoracic cavity. The conventional Finochietto retractor achieves this by anchoring onto soft tissue surrounding the ribs—directly impinging the intercostal nerve, which runs along the inferior rib margin under the costal groove.

Key consequences:
- 57% of patients develop PTPS, often with severe neuropathic pain
- Chronic pain contributes to reduced mobility, prolonged opioid use, and delayed recovery
- PTPS adds >$2,500 per patient in downstream healthcare costs and increases indirect costs from readmissions and long-term complications
Critically, existing solutions attempt to manage force, not eliminate nerve contact. No widely used device addresses the underlying mechanical cause of nerve injury.
Design Rationale
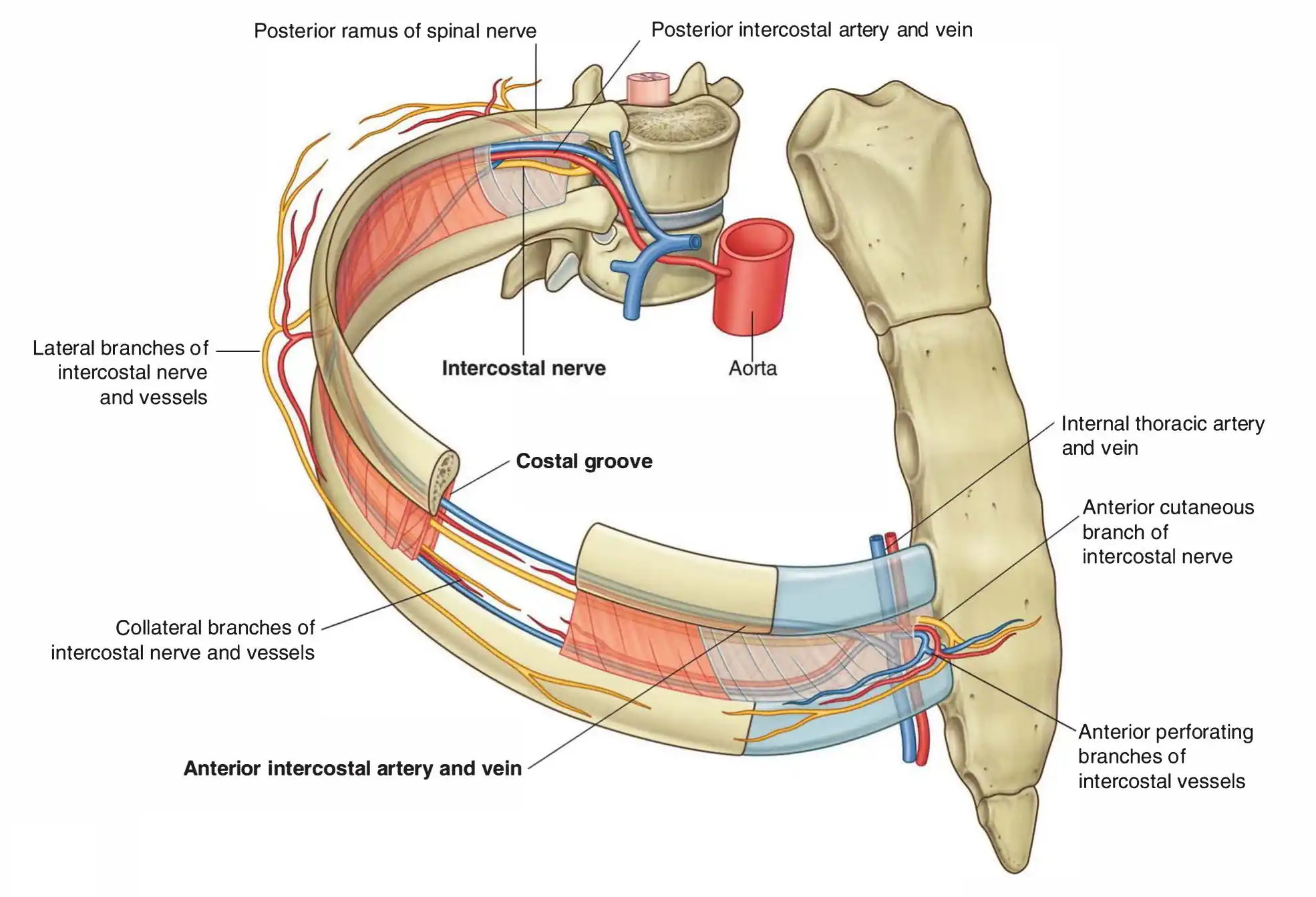
Through literature review and interviews with thoracic surgeons, we identified a critical and underutilized insight:
Thoracotomies already require drilling holes in ribs for suturing.
Rather than compressing tissue between ribs, these pre-existing intracostal holes can serve as structural anchor points for retraction. This reframing led to a fundamentally different approach:
- Shift force application from the intercostal space to the rib interior
- Use bone—not soft tissue—to carry retraction loads
- Eliminate direct contact with the intercostal nerve altogether
The Solution
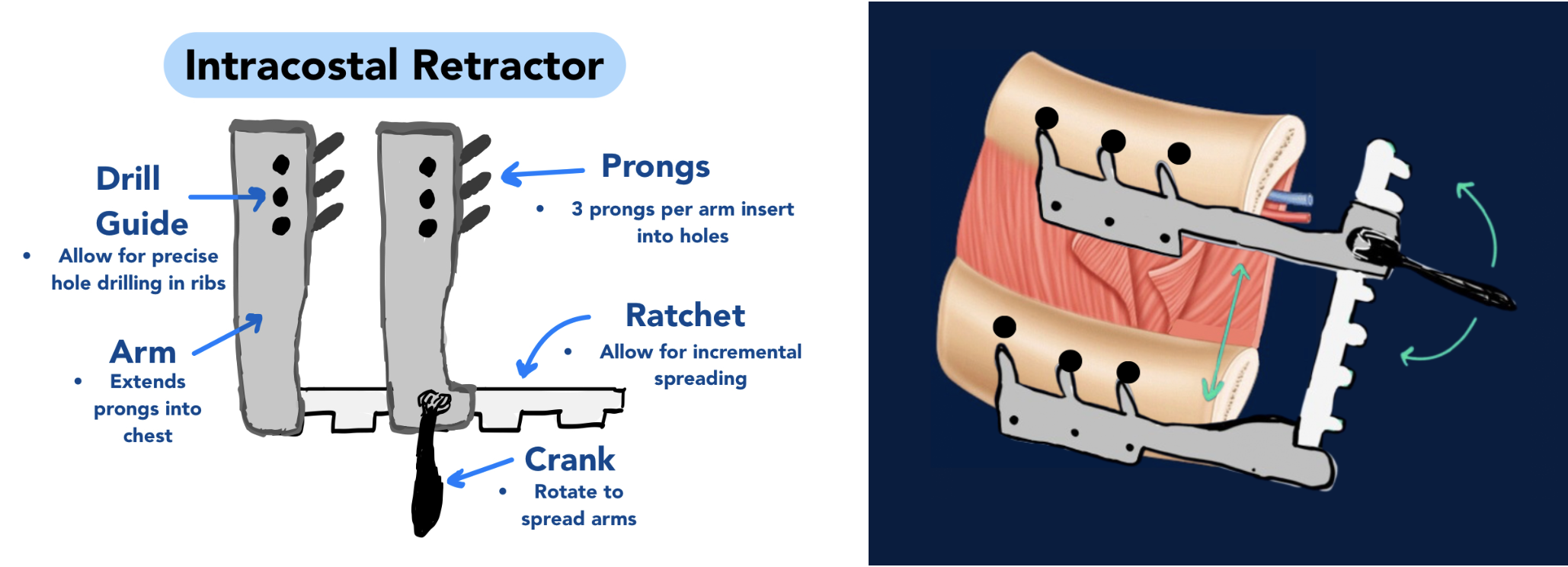
We designed a nerve-sparing intracostal rib retractor that applies force through intracostal prongs inserted into drilled rib holes, rather than compressing tissue between ribs.
Core innovations
- Intracostal prong anchoring: retractor arms engage the interior of the ribs, avoiding the intercostal nerve bundle
- Use of existing surgical workflow: leverages rib holes already drilled for sutures, adding no fundamentally new surgical trauma
- Precision drill guide: ensures consistent hole spacing and alignment, minimizing fracture risk and improving reproducibility
- Modular and scalable design: compatible with open thoracotomy and adaptable to future minimally invasive or robotic workflows
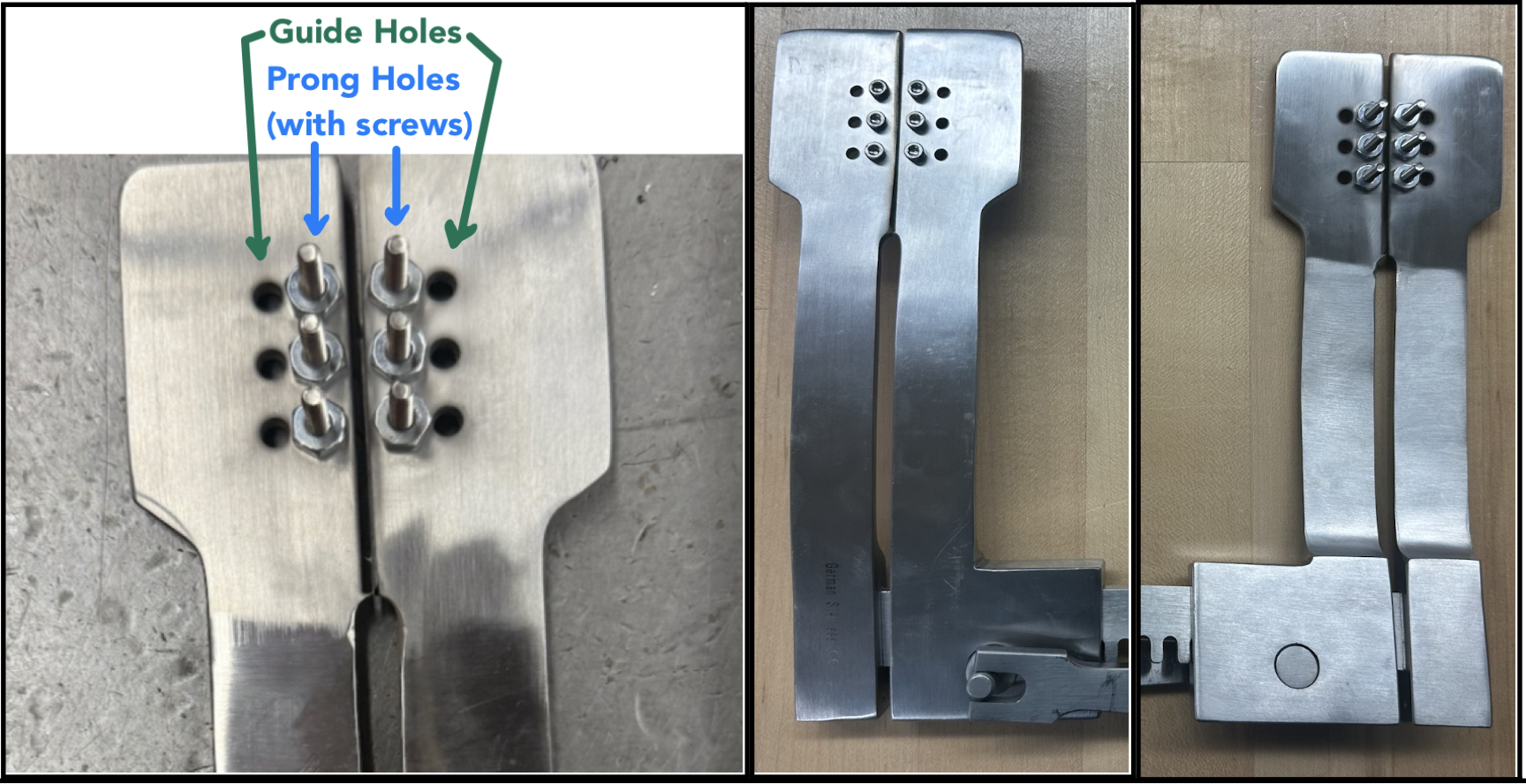
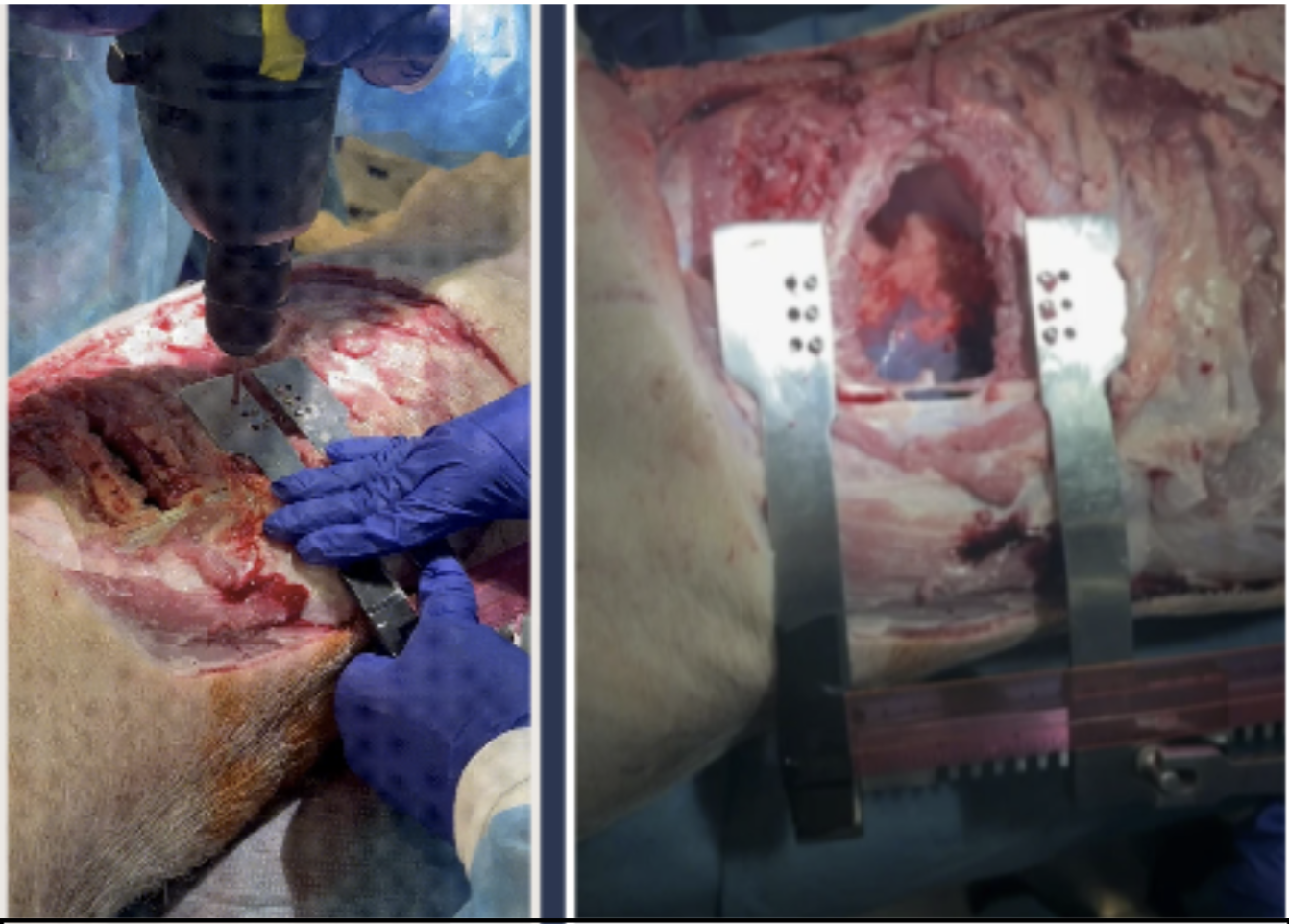
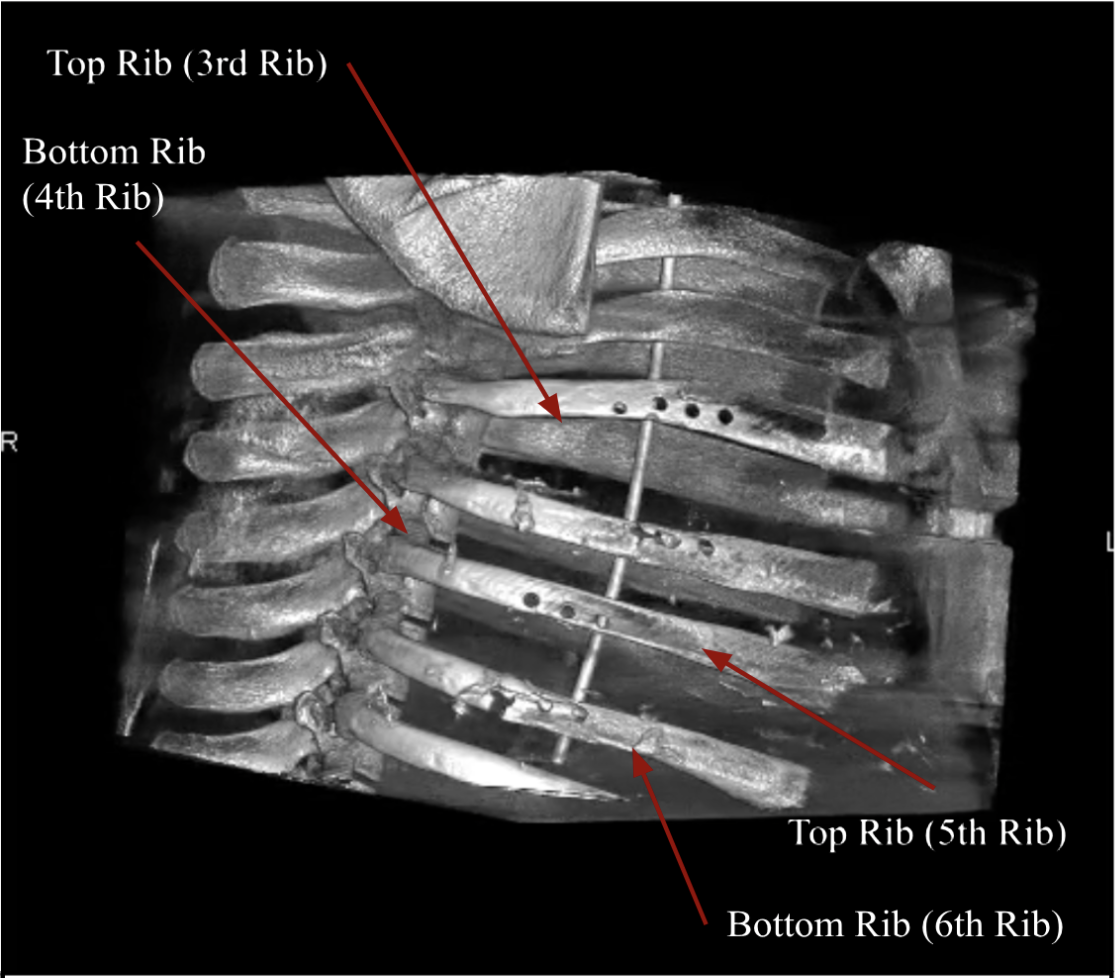
Final Prototype (Figures 1.5a–d)
Impact & Significance
By eliminating direct intercostal nerve compression, this retractor has the potential to:
- Dramatically reduce PTPS incidence
- Improve postoperative mobility and respiratory recovery
- Reduce long-term opioid dependence
- Lower hospital readmissions and total cost of care
- Improve patient experience in one of the most painful surgical procedures
With an estimated 66,000 open thoracotomies annually in the U.S., even modest reductions in chronic pain rates translate into thousands of patients spared lifelong neuropathic pain and large downstream cost savings.
Looking Forward
Preclinical testing revealed clear nerve-sparing benefits alongside opportunities for mechanical refinement. A proposed hybrid design—intracostal anchoring on the upper rib with a conventional blade on the lower rib—offers a promising path to balance nerve protection with fracture resistance.
With further optimization and 510(k) regulatory clearance, this device represents a first-in-class retraction strategy—one that addresses the root cause of post-thoracotomy pain rather than its symptoms.
Key Skills Demonstrated
- Clinical needfinding & surgeon interviews
- First-principles biomechanical design
- Translational medical device innovation
- Regulatory and reimbursement strategy
- Preclinical validation & design iteration